
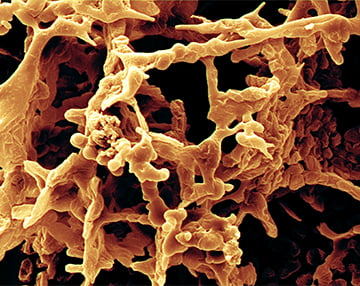

Bacteria colonize surfaces and establish a sessile mode of growth in biofilms, heterogeneous matrices of extracellular polymeric substances (EPS). Microbial biofilms are implicated in chronic infections and are more resistant to antimicrobial agents and the immune system than their planktonic counterparts. Microorganisms in most habitats in/on the human body are believed to grow predominantly as sessile polymicrobial communities encapsulated in biofilms. Researchers at Oak Crest have been actively studying clinical biofilm specimens associated with a wide range of conditions ranging from middle ear infections to bacterial vaginosis. The research involves characterizing the physicochemical properties of the EPS. For example, we have shown that two distinct phenotypes are characteristic of the complex microbial communities colonizing intravaginal rings in non-human primates and women. We continue to study the genetic mechanisms that link biofilm structure, composition, and properties and link these with community composition to host responses.
In related work, researchers at Oak Crest are investigating the impact of sub-lethal exposure of bacterial communities to antibiotics, with a focus on biofilm formation. Efforts to date have focused on laboratory monocultures of Haemophilus influenzae, a human respiratory tract pathogen. We are expanding these activities by linking results from laboratory studies with analyses of clinical specimens from patients suffering from middle ear infections and chronic sinusitis.
